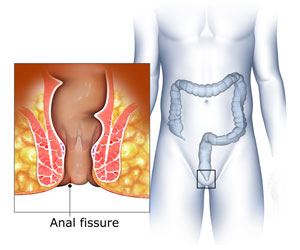
What is an Anal Fissure?
The anus is the last part of the digestive tract and is lined with contracting muscles that control the removal of stools. An anal fissure is a tear in the tissue lining the anus and is associated with pain and bleeding during bowel movements. It can occur in almost anyone, however, it is more commonly seen in infants.
An anal fissure can be caused because of trauma or injury to the anal canal while passing hard or large stools, constipation, or straining during bowel movements or childbirth. It can occur independently or in association with other conditions like chronic diarrhoea, HIV, anal cancer, tuberculosis, syphilis, and herpes. Sometimes, excess stress on the two muscular sphincters (rings) that control the anus can reduce blood supply and lead to the development of an anal fissure.
Depending on its severity, anal fissures can be acute or chronic. Anal fissures can be superficial or shallow, making their detection difficult. Therefore, a visual inspection may not suffice at all times. In most patients, an anal fissure heals on its own in a few days or weeks (acute), but in cases when it doesn't heal even after 6 weeks (chronic), medical treatment or surgery may be recommended.
What are the Signs & Symptoms of Anal Fissure?
The typical symptoms of an anal fissure include pain during and several hours after a bowel movement. Even though the tear caused by an anal fissure is small (about 1cm), the condition is painful and may persist for an hour or more after passing faeces. The severe pain may make patients apprehensive to the point of avoiding defecation, which further aggravates the condition. Pain is usually more intense in acute anal fissure.
Other symptoms include:
- Blood in the stools, on the toilet tissue or in the bowl
- Muscular spasms at the end of the anus
- Cracked or ripped anal skin
- Itchy fissures
- Yellow discharge that has an unpleasant odour
Chronic anal fissures can grow deeper into the tissue and form ulcers, which can further delay the healing process.
What are the methods of Screening & Diagnosis of Anal Fissure?
Your doctor will review your medical history and conduct a physical examination of the anal region. Most anal fissures can be diagnosed by viewing the anal region on separating the buttocks. If the tear is visible, diagnosis becomes easy and treatment can be started immediately. If not, a sample of the rectal tissue may be removed for examination.
Anal fissures can be diagnosed by digital rectal examination or using an instrument called an anoscope. The digital rectal examination involves inserting a gloved finger into the anal canal. The anoscope is a short instrument with a lighted tube that can help your doctor view and examine the fissure. If these procedures cause extreme pain, your doctor may wait till the fissure heals or use a topical anaesthetic to reduce the discomfort.
Your doctor will have to rule out other problems that can cause fissures. Anal fissures are characteristically located either on the back or front surfaces of the anus. If your condition is characterized by several fissures, or the fissures are located on the sides of the anus, then you may be suffering from a different condition (inflammatory bowel disease, anal cancer, syphilis or HIV infection). Your doctor will conduct further tests to confirm these conditions.
What are the Treatment Options for Anal Fissure?
The treatment measure adopted would depend on the nature of the fissure, i.e. if it is acute (lasting up to a few days) or chronic (lasting for more than 6 weeks).
Home remedies such as increasing the intake of fibre and fluids are highly recommended for softening the stools. Foods rich in fibre, like whole-grain bread, fruits, and vegetables, brown rice, and oats, can help heal anal fissures in a few weeks.
Your doctor may also advise you to soak the anus in warm water for 10 -20 minutes as often as possible, particularly after bowel movements, to relax and reduce the stress on the sphincter muscles. Steroid creams, other topical applications, and Botox injections may be prescribed to reduce discomfort, improve blood circulation and relax the sphincter muscles of the anus.
Topical anaesthetics and pain medication may be prescribed to control pain.
Surgery is usually the last resort when other treatments do not provide the needed relief. Some of the surgical procedures include:
- Lateral internal sphincterotomy: Your doctor may perform lateral internal sphincterotomy, where pain and spasm are reduced by removing a small section of the anal sphincter muscle.
- Fissurectomy: Your doctor will surgically remove the anal fissure with the surrounding healthy tissue. This method is not commonly used in adults but is performed mostly in children.
- Advancement anal flaps: Your doctor will take healthy tissue from a different part of the body to repair the fissure and help improve blood flow. This method is commonly used to treat chronic fissures that have occurred due to injury to the anus, especially after pregnancy.